OXFORD, UK – 4 December 2025 – PrecisionLife today announced new findings from the most detailed genetic analysis of myalgic encephalomyelitis (ME, also known as ME/CFS) ever conducted, revealing more than 250 core genes associated with the disease, including 76 genes linked with long COVID, and uncovering dozens of drug repurposing opportunities supported by genetic biomarker tests, offering potential for faster and lower-risk routes to developing targeted treatments.
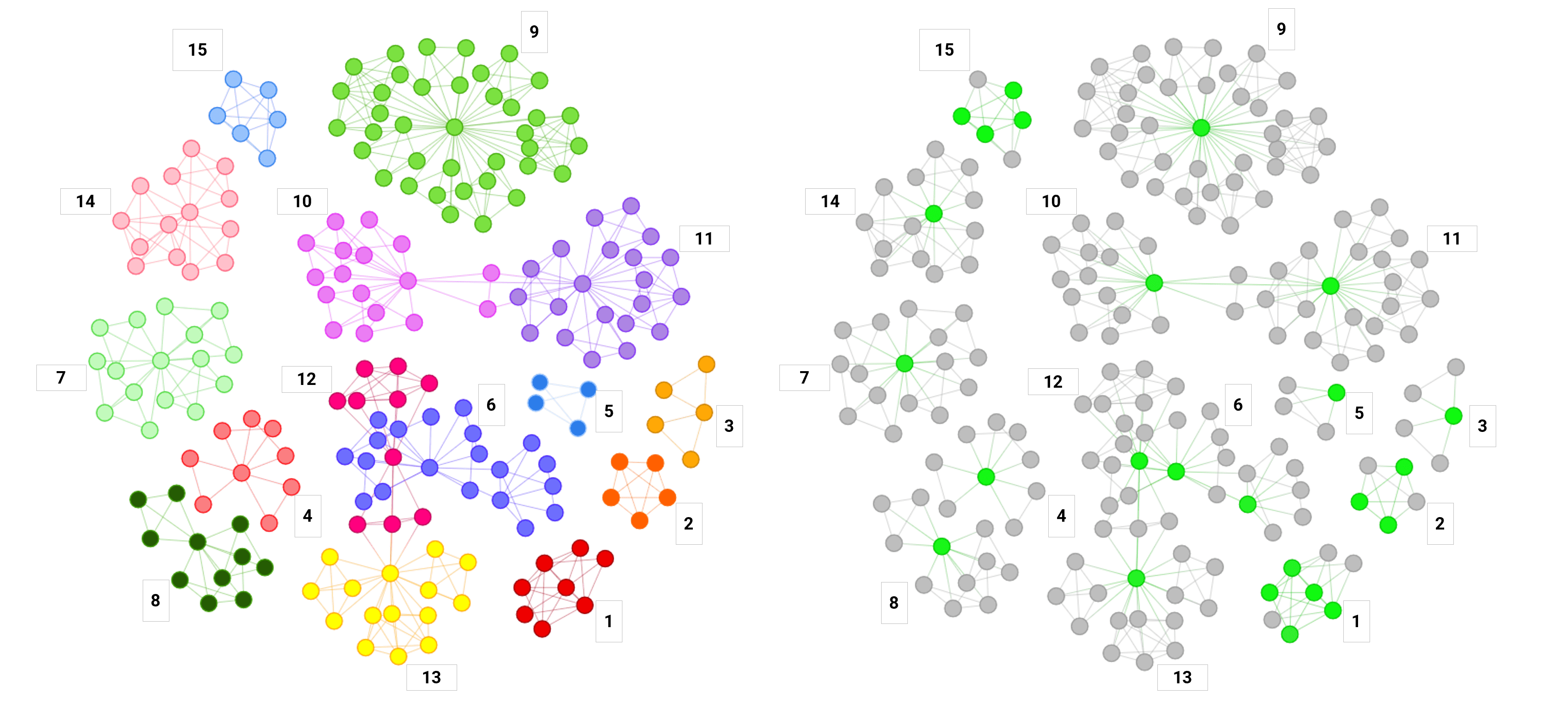
The study, now available as a pre-print and submitted for peer review, applied PrecisionLife's AI-led combinatorial analytics platform to analyze genomic data from two DecodeME cohorts together with UK Biobank to confirm reproducibility of results across three independent datasets. The analysis identified 7,555 genetic variants (including the 8 identified by the recent DecodeME GWAS study ), that were consistently associated with increased disease risk in three different populations.
These results confirm that ME is a deeply polygenic and biologically heterogeneous condition with at least four major disease mechanisms implicated by genetic signals: neurological dysregulation, inflammation, cellular stress response, and calcium signaling.
The findings have important implications for the future of ME research and treatment. They reinforce the need for a stratified approach, with genetic evidence pointing to multiple biological subgroups within the disease. This means that future clinical trials are likely to be more successful when they target specific patient subtypes rather than treating ME as a single, uniform condition. This also aligns closely with the lived experience of many people in the ME community, who have long recognized the diversity of symptoms and disease patterns.
The study also demonstrated a strong genetic overlap between ME and long COVID, with 76 of 180 genes previously linked to long COVID also significantly associated with ME in the DecodeME dataset. This indicates that ME and long COVID are overlapping but different conditions, where their shared biological pathways offer promising potential for developing drug therapies that could successfully treat patients with either condition.
To support global research efforts, PrecisionLife has published the full list of SNPs and genes identified in this analysis, enabling academic groups, clinicians, and biopharma researchers to accelerate drug repurposing studies, target discovery, and development of new mechanism-based therapies.
ME and long COVID together affect an estimated 400 million people worldwide, contributing more than $1 trillion annually to healthcare costs and lost economic productivity . The lack of diagnostic tools, effective treatments or biological clarity on its causes has contributed to decades of unmet need for patients, and prolonged underinvestment in development of research and healthcare pathways.
Dr Steve Gardner, CEO of PrecisionLife:
“These results reinforce that ME has a clear biological and genetic basis and is a complex multisystemic disease. ME is highly polygenic and heterogeneous, so no single drug will help everyone. Stratifying patients by the mechanisms that are driving their disease will be essential for predicting who will benefit from which therapies and for developing accurate diagnostic tests. We’re beginning to have this level of insight, and we hope that in the future the genetic biomarkers we’ve identified for existing and new drug repurposing candidates could help make trials with collaborators worldwide more successful.”Sonya Chowdhury, CEO of Action for ME:
“These findings offer further hope to people with ME around the world. For decades, people affected by ME have lacked recognition, access to proper diagnosis and effective treatments. PrecisionLife’s results represent a major step forward in understanding the biology of the disease and provide real opportunities for targeted therapies to move into clinical testing. We are proud that DecodeME has helped pave the way for this progress, and we will continue to champion research that delivers meaningful benefits for the community.”Prof Chris Ponting, Chair of Medical Bioinformatics at the Institute of Genetics and Cancer, University of Edinburgh, and investigator on the DecodeME study:
“DecodeME was designed to reveal the complex genetics of ME by providing a dataset of the scale and quality required for robust discovery. PrecisionLife has shown how making such datasets available can quickly generate new insights into ME disease biology. This is an exciting outcome of making consented DecodeME data available to research partners and we look forward to enabling further future collaborations.”Helen Baxter, Patient Advocate & Patient and Public Involvement Representative:
“These results greatly enhance our understanding of the biology of ME and present opportunities for drug repurposing which affords hope to the millions of people living with ME and long COVID around the world.”
The research forms part of the LOCOME (LOng COvid and Myalgic Encephalomyelitis) program, led by PrecisionLife and funded in part by Innovate UK. The LOCOME program was delivered in collaboration with Action for ME and the University of Edinburgh.
The LOCOME partners are especially grateful to the tens of thousands of people with ME who contributed their data to DecodeME, often whilst experiencing pain, fatigue, and brain fog.
This work uses also data provided by patients and collected by the NHS as part of their care and support, for which we are also grateful.The partners also wish to thank the patient and public involvement (PPI) representatives on LOCOME, whose insight and lived experience helped shape the delivery and direction of this project.
We hope the findings published today will encourage biopharma, clinical researchers, and academic groups to work together to advance repurposing candidates into targeted clinical trials, supported by mechanistic biomarkers that can identify those patients most likely to respond.
Read the full study paper here: precisionlife.com/locome-preprint
About PrecisionLife®
PrecisionLife is a precision medicine company transforming how we predict, treat, and prevent complex chronic diseases. Using our proprietary AI-driven combinatorial analytics platform, we uncover the biological drivers of disease at unmatched scale and resolution - personalizing risk prediction, accelerating diagnosis, and optimizing treatment decisions.
Our unique ability to stratify patients by underlying disease mechanisms supports a broad range of solutions, including diagnostic and prognostic testing, differential triage, treatment optimization, clinical trial enrichment, and drug repurposing.
PrecisionLife partners with healthcare providers, payors and biopharma innovators to deliver clinically actionable insights that improve health outcomes, reduce costs, and extend healthy lifespan for billions of people affected by chronic disease.