Patient Stratification of UK Biobank Asthma Population Reveals Distinct Genetic and Mechanistic Differences between T2-High and T2-low Asthma Endotypes
Asthma can be split into two major endotypes (T2 high and T2-low) characterised by distinct molecular drivers. The genetic risk factors and underlying pathology of T2-low asthma are less well-characterised than the T2-driven endotype and there is no clear consensus on the clinical definition, although patients with low eosinophil counts often display a greater proportion of neutrophilic inflammation.
Standard GWAS-based approaches aiming to uncover common mechanisms across different disorders are limited to identifying single variants with high prevalence. The key to understanding complex, multi-symptomatic diseases influenced by multiple genetic loci, epidemiological and/or environmental factors is to find combinations of these factors in sub-cohorts with distinct characteristics.
The PrecisionLife platform utilises a hypothesis-free method for the detection of combinations of features that together are strongly associated with variations in disease risk, progression rates and other clinical phenotypes often observed in patient subgroups. Resulting patient stratification insights allow us to identify mechanistic subgroups shared by different indications.
We aimed to identify genetic differences between the two cohorts and further characterise the biological drivers of T2-low asthma. We selected two subsets of asthma patients using blood eosinophil data from the UK Biobank to investigate the genetic differences between patients with T2-high and T2-low asthma. PrecisionLife analyzed genotype data from each asthma case population against healthy controls to compare the genetic drivers underlying the two asthma endotypes. A pathway enrichment analysis was conducted to evaluate the differences in the biological pathways associated with the genetic variants identified with each cohort.
Results
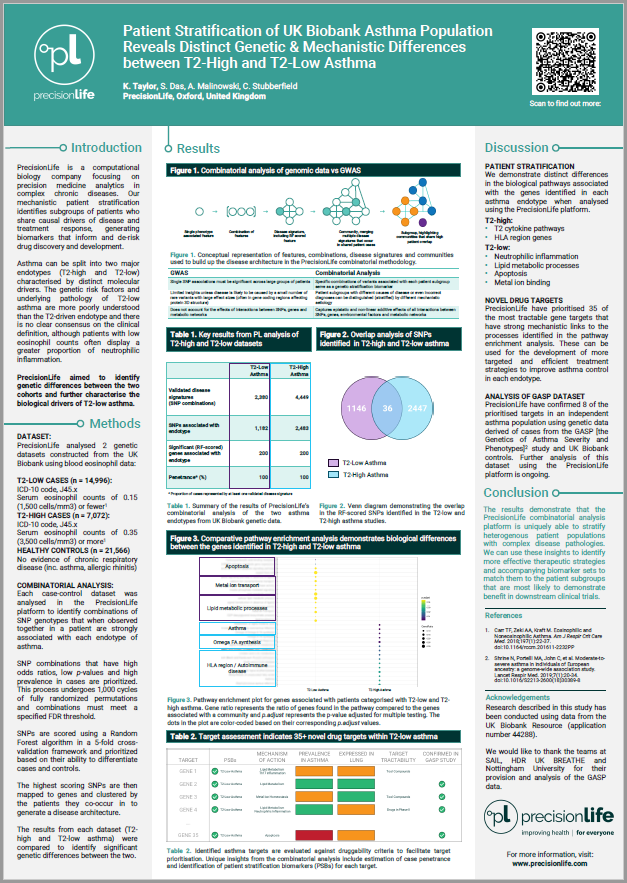
The PrecisionLife platform identified 2,483 SNPs that were highly associated with T2-high asthma and 1,182 SNPs in the T2-low cohort. When the SNPs were compared, only 36 were common between the two datasets. A comparative pathway enrichment analysis further indicated that the differences in SNPs found in the two asthma cohorts related to clear differences in biological processes underpinning the different endotypes.
Many of the genes associated with the T2-high population are key regulators of the T2-driven immune pathways associated with allergic asthma, whereas patients with T2-low asthma demonstrated combinations of genetic variants associated with the biological pathways such as apoptosis, metal ion binding and lipid metabolism.
Conclusion
A greater understanding of the mechanisms causing the pathology of T2-low asthma used for the development of more targeted and efficient treatment strategies may improve asthma control in this population. PrecisionLife are currently working to replicate and validate these insights using an additional asthma cohort derived from the GASP study.
Asthma disease study
For more information on our research into the mechanism-based stratification of T2 and non-T2 asthma, view our disease study, the findings of which hold significant potential for better patient stratification, diagnostic biomarkers, and new treatment options.
Find out more